How is MS diagnosed?
Multiple Sclerosis is diagnosed by a combination of clinical, radiological and biochemical findings. There is no one marker that confirms or rules out the diagnosis of MS. Patients therefore usually goes through a variety of investigations before the diagnosis of MS can be made. The following are what you would expect to undergo if you are suspected to have MS.

History and Clinical Exam
Clinical history is very important in the diagnosis of MS. The onset, duration and nature of your symptoms all help to differentiate whether you are likely to suffer from MS or other types of neurological diseases. Sometimes, you may have had symptoms in the past which you did not pay attention to, but would help a doctor determine if you have genuine MS. Clinical examinations would also sometimes reveal symptoms or signs that you were not aware of, and prompt further investigations below.
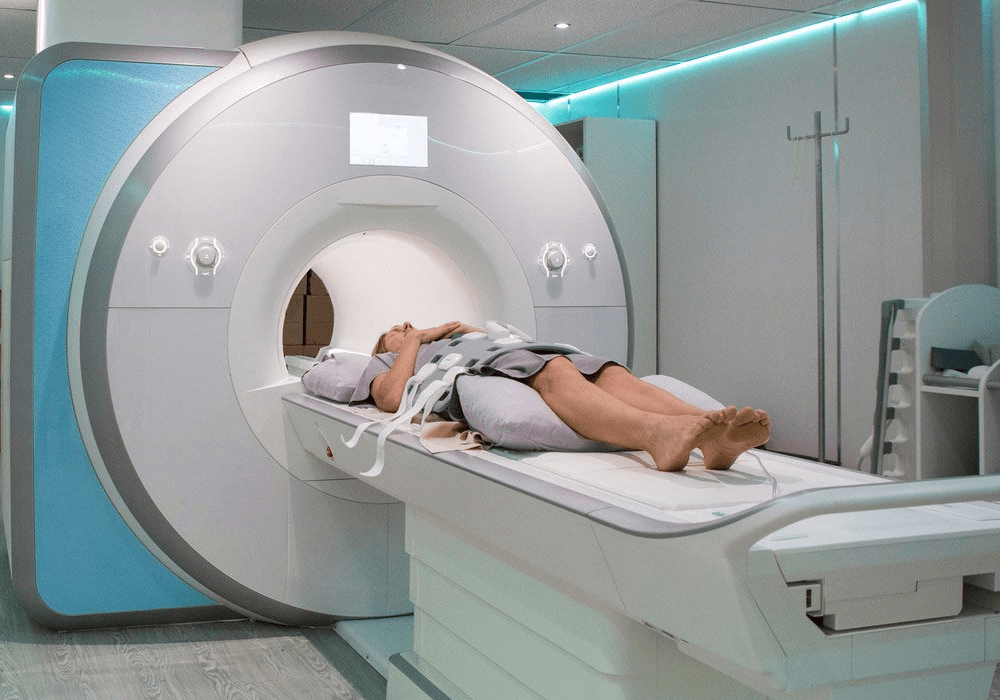
Magnetic Resonance Imaging (MRI)
Magnetic Resonance Imaging (MRI) is the most useful radiological examination for MS, not only for diagnosis but for disease monitoring. In MS patients, MRI of the brain and spine may reveal areas of ‘white spots’, which are demyelinating plaques indicating disease activity. Unless there are reasons that make you unsuitable for contrast injection, doctors would usually order contrast MRIs because they can signify whether a plaque is active, which implies a recent attack. An MRI of the orbits are sometimes arranged as well to look at the optic nerves, which are responsible for your vision. Computed Tomography (CT) is usually normal and not helpful in the diagnosis of MS.
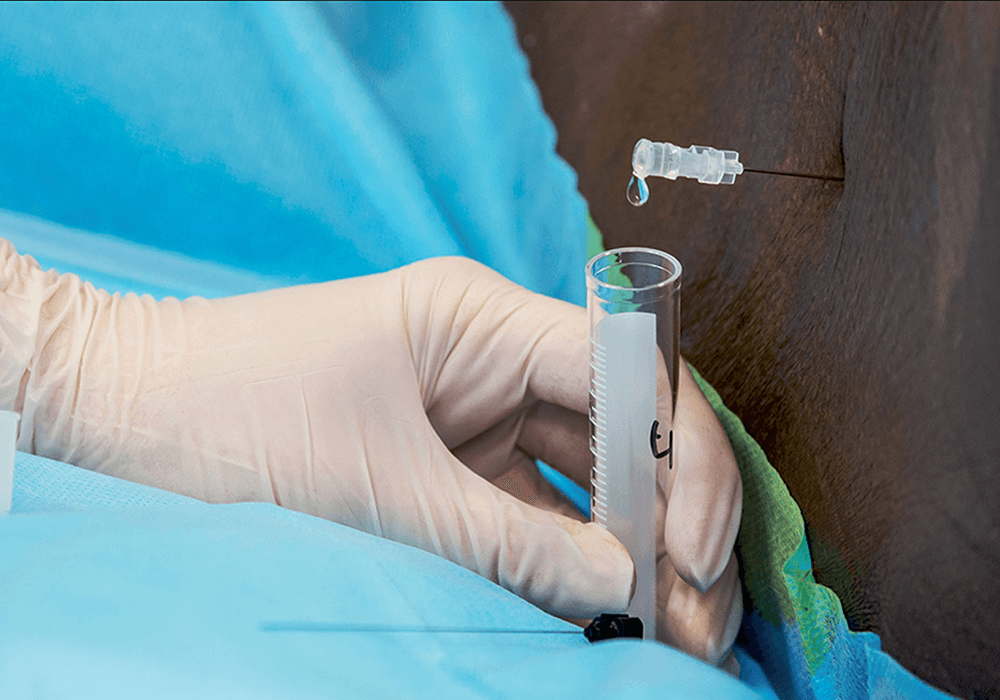
Lumbar Puncture (LP)
Some MS patients have an abnormal protein called oligoclonal bands in their cerebrospinal fluid (CSF), which is the liquid that coats your brain and runs in your spinal cord. Lumbar
puncture is an investigation where a needle is inserted between your spinal columns to gain access to the CSF space. A small amount of CSF is drawn for testing of the oligoclonal bands in addition to ruling out other diseases such as infection.

Blood Tests
While there is no single blood test that can confirm the diagnosis of MS, they are still important to exclude other conditions which may mimic MS. In particular, Neuromyelitis Optica Spectrum Disorder (NMOSD) and Myelin Oligodendrocyte Glycoprotein Antibody-associated Disease (MOGAD) are very similar to MS but has drastically different treatment. It is also far more prevalent in the south-eastern Asian countries compared with the rest of the world. Patients suspected to have MS should have the anti-NMO and anti-MOG antibodies tested as part of their workup.
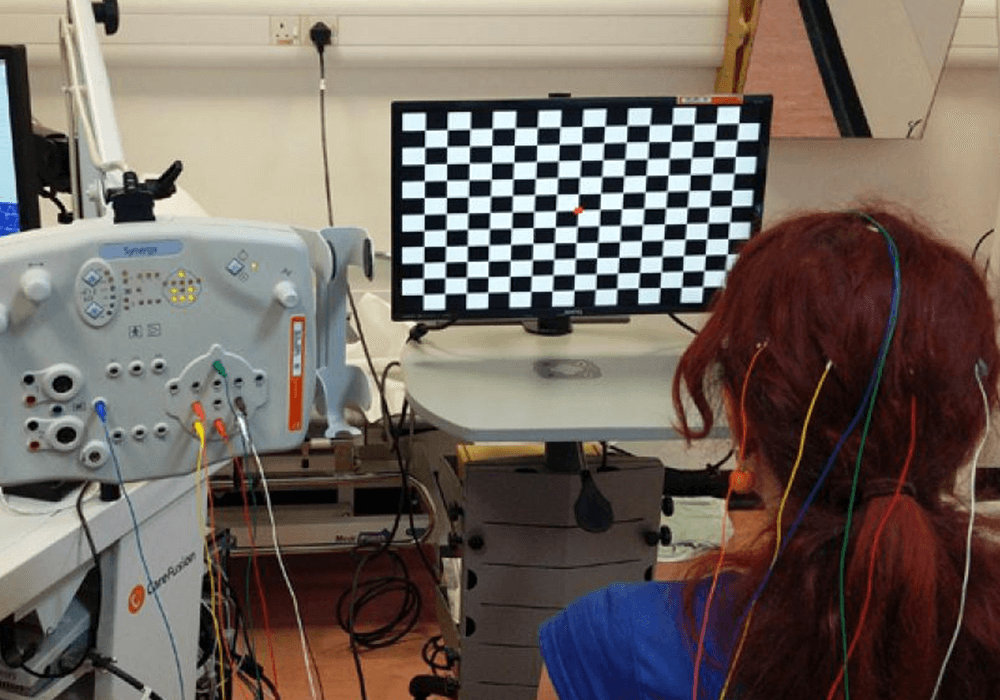
Evoked Potential Studies
Evoked potential studies are neuro-physiological tests that use electric signals to examine the neuro-pathways in your body. While they are less performed nowadays due to advances in other investigation techniques, they still have a role in certain conditions. For instance, visual-evoked-potentials are still performed to test the optic nerves, which may not be seen well on MRI.
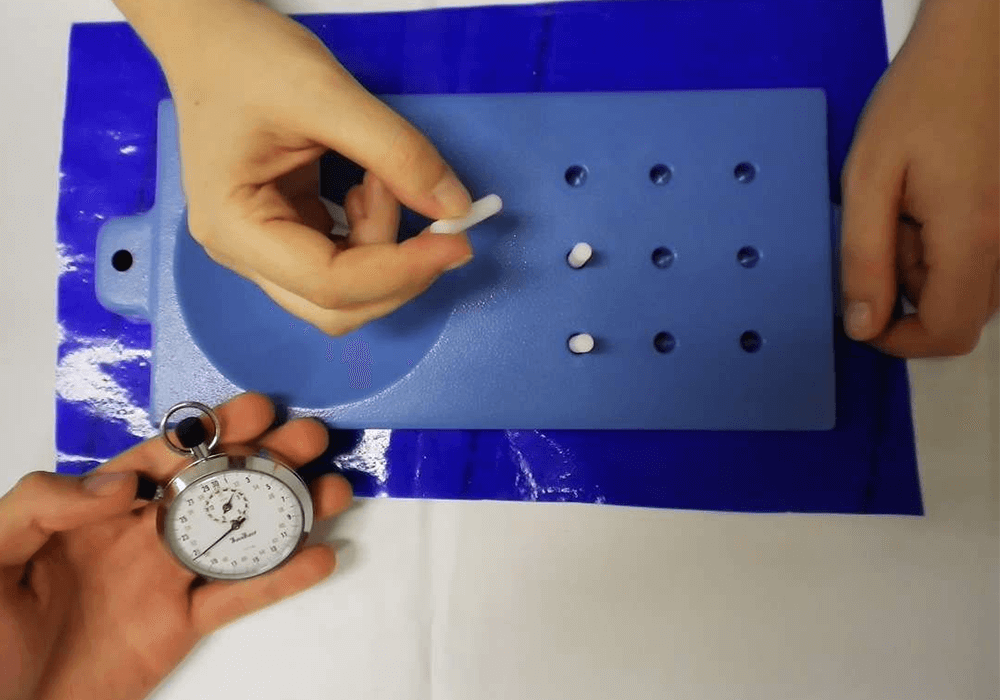
Functional Assessments
While MRI is the most important means to monitor disease activity of MS, there are several assessment tools such as 9-hole Peg Test, 25-foot Walk and Symbol Digit Modalities Test that can provide valuable information on patients’ functional status. They allow doctors to monitor patients’ cognition, upper limb and lower limb functions.
Others
Depending on your symptoms, doctors may sometimes arrange additional tests for you, or refer you to specialists such as Ophthalmologists to perform specific tests on your eyes. Consult your doctor if in doubt, and remember not to jump to conclusions simply because one of your investigations is abnormal!




