What is MS?
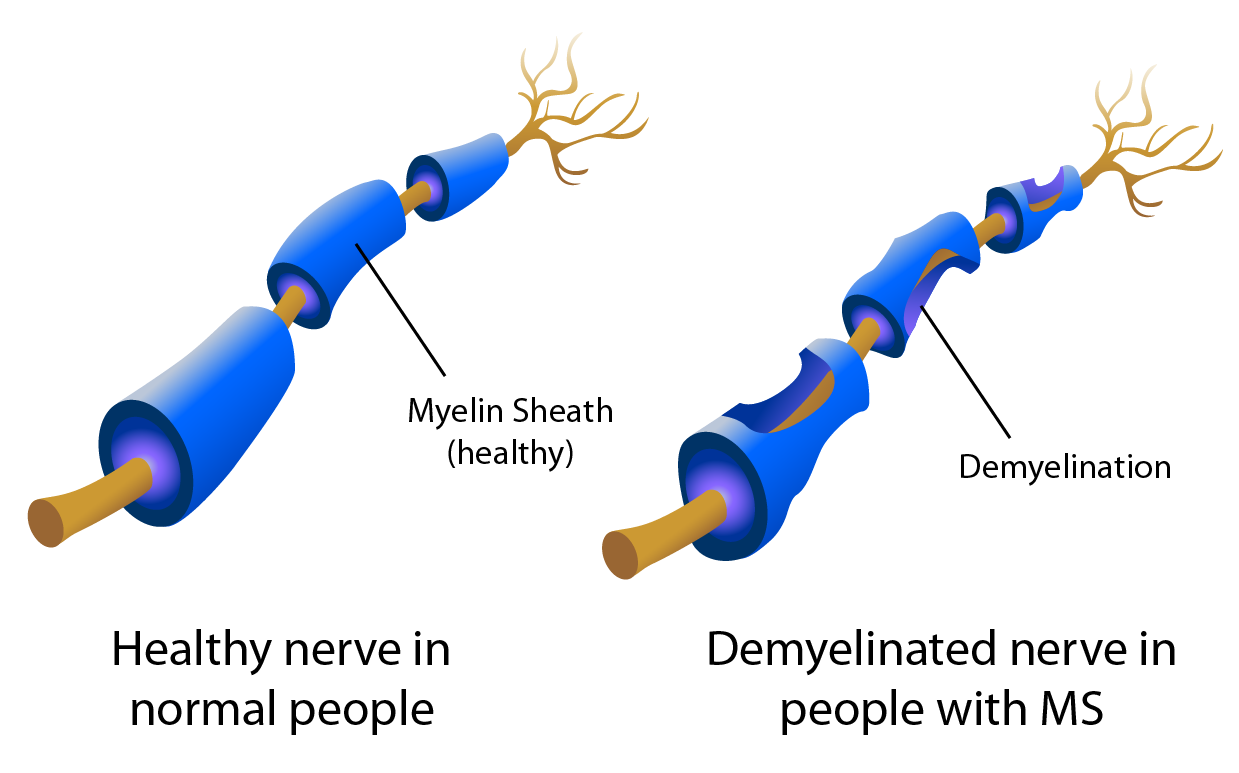
Multiple Sclerosis (MS) is a disease that affects the central nervous system, which mainly consists of the brain, spinal cord and eyes. In the human body, nerves (especially axons) are surrounded by an outer layer called myelin, which is important for nerve conduction. This is similar to how electrical wires are protected by a plastic outer layer. In MS, this layer of myelin is damaged, in a process known as ‘demyelination’.


Demyelinated nerves result in slowing of nerve conduction, and lead to a variety of symptoms depending on the location of damage. Although the body attempts to repair these demyelinated nerves, scar tissues known as ‘plaques’ are often formed, which unfortunately do not return the nerves to normal functioning. Multiple Sclerosis received its name from these ‘hard’ and ‘sclerosed’ plaques, which can occur anywhere in the central nervous system in a ‘multiple’ manner.
With each attack, the body’s ability to repair the demyelinated nerves decreases. As ‘plaques’ accumulate, the disease burden stacks up, and patients may eventually suffer from irreversible disability.
What causes MS?
Although MS has been recognized for more than a century, its exact mechanism remains uncertain. However, it is believed to be autoimmune in origin, which means that the human body’s immune system is wrongly targetting the nerve myelin, leading to inflammation and damage.
A genetic origin has been suggested, but so far no definite genetic markers have been identified. It is also believed that environmental factors may contribute to MS, since areas with higher latitudes appear to have higher prevalence of MS.
How common is MS and who gets affected?
According to data from the World Atlas of MS which was mapped out by the Multiple Sclerosis International Federation, as of 2020, the global median MS prevalence was 35 per 100,000, with an incidence of 4 per 100,000. The prevalence of MS appears highest in North America and Europe, affecting approximately 1 in 2000 people.
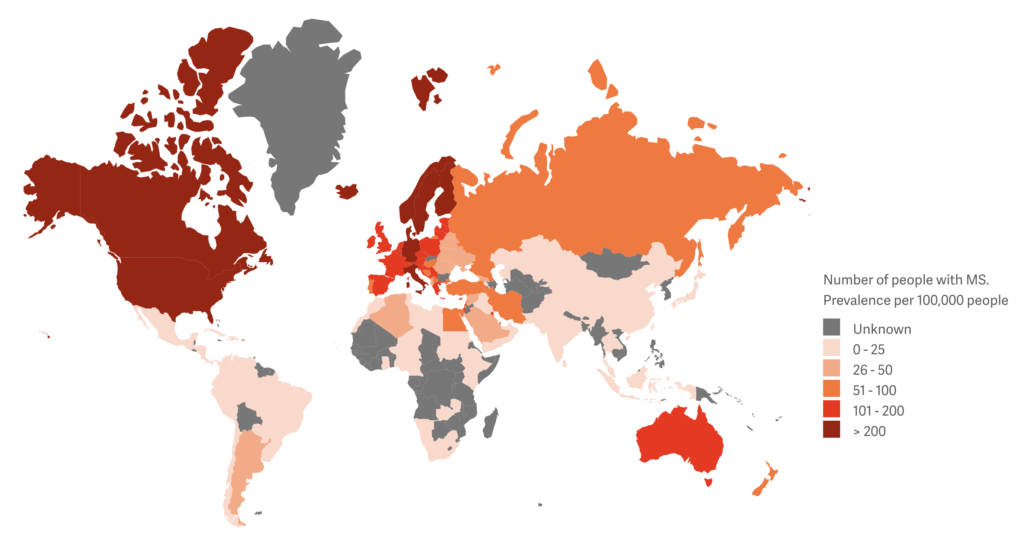
In Hong Kong, a recent local publication calculated the prevalence of MS in at-risk population (excluding persons 60 years old or above) to be 6.9 per 100,000 in 2020. In the past, Hong Kong was thought to be a region of low MS prevalence. However, the updated figure suggested that MS prevalence in Hong Kong was similar to other Asian regions. Between 2013 and 2020, the age-standardized incidence of MS in Hong Kong was 0.86 per 100,000 population-years in adults, and 0.16 per 100,000 in the paediatric group.
In Hong Kong, the male to female gender ratio of MS patients was approximately 1:3. The mean age of disease onset was 27-33, which echoes international findings that MS primarily affects people between the age of 20 to 40.
What are the different types of MS?
In 2013, the American Academy of Neurology published an updated classification system for multiple sclerosis, defining MS into 4 major types:
Clinically isolated syndrome (CIS)
CIS refers to the first clinical attack of a disease highly suggestive of multiple sclerosis, but does not fully fulfil the diagnostic criteria yet. Some patients remain as CIS and never experience a second attack throughout their lives.
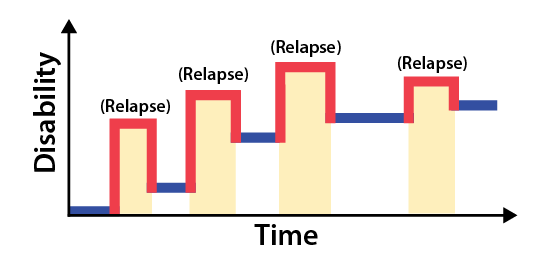
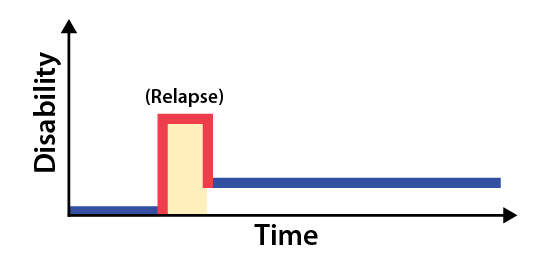
Relapsing-remitting MS (RRMS)
RRMS is by far the commonest form of MS. Patients with RRMS suffers from repeated ‘relapses’, after which the symptoms will improve and enter the ‘remission’ phase. However, as mentioned above, the damaged nerves may not fully recover, and disability still accumulates with repeated attacks. Most available MS treatments are targeted at RRMS, which aims to prevent relapses in order to reduce disability accumulation.
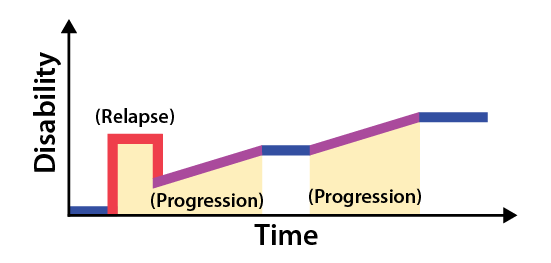
Primary progressive MS (PPMS)
PPMS is a progressive form of MS where patients experience gradual deterioration after the first attack despite lack of relapses.
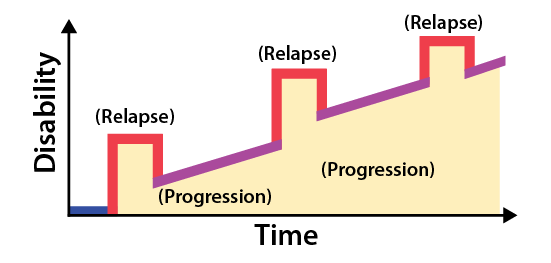
Secondary progressive MS (SPMS)
SPMS is also a progressive form of MS but patients suffer from clinical relapses in addition to a gradual deterioration. SPMS has been suggested to be poorly controlled or late form of RRMS where patients accumulate disability much quicker than their bodies can regenerate.
